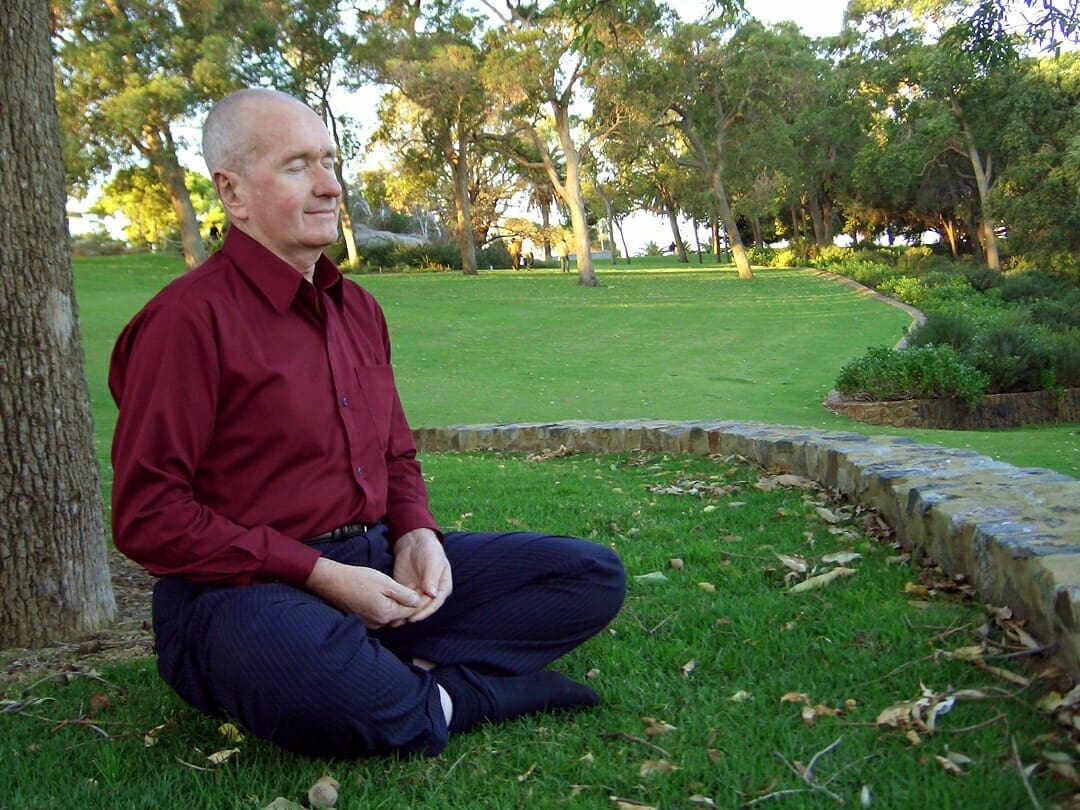
For thousands of years, yoga has stood as one of the most important practices for spiritual discipline and transcendence of the ego. But today, yoga has made its way from out of the ashrams and into multiple neurological institutes and research centers throughout the world, being investigated as a new treatment approach to some of today’s most complicated neurophysiological conditions.
Already, this meditational exercise has been shown to help treat a broad spectrum of conditions — depression, anxiety, stress, post-traumatic stress disorder, and attention deficit hyperactivity disorder. Yet one of the most exciting and new breakthroughs in the fields of contemplative neuroscience and aging is how yoga modulates the brains of Alzheimer’s patients and those at risk for developing it later in life.
As biomedicine and technology advance, people are living longer. Since 1840, the average lifespan has more than doubled and is increasing at the rate of about five hours per day. While some see this as biomedical progress, others see it as a warning. Dr. Gregory Petsko — an internationally renowned biochemist and member of the National Academy of Sciences — predicts that by 2050, there will be about 32 million people living in the United States over the age of 80 and about half of them will have Alzheimer’s. Today, the disease already stands as one of the most challenging public and global health concerns — the Alzheimer’s Association estimates that, as of 2016, 5.4 million Americans of all ages are afflicted.
Even though billions of dollars are being spent on Alzheimer’s medical care and clinical research, it still stands among the top 10 causes of death in America that cannot be effectively prevented, cured, or even slowed. Both the financial and emotional burden upon family members who act as caregivers for loved ones with Alzheimer’s disease can cause them to be six times more likely to develop dementia than a noncaregiver. The inadequacy of effective pharmaceuticals and severe stressors placed upon families, patients, and doctors have expanded Alzheimer’s research into the field of integrative care; a field which can utilize both mind-body practices and medications to optimize clinical care.
Yoga may be one of the most beneficial mind-body practices that can be administered to this patient group. In order to understand how the practice of yoga may be a successful complementary means for treating age-related cognitive decline and Alzheimer’s disease, one must look at the specific neural systems that may be targeted and nurtured during this practice. Even though the World Health Organization officially began promoting yoga in developing countries as early as 1978 as a therapeutic practice, neuroscience researchers remained unsure about whether yoga held any promises for treating some of the world’s most complicated neurological diseases.
A groundbreaking meta-analysis was published by neurologist Dr. Shri Mishra and his fellow researchers. They gathered studies from numerous databases — PubMed, Ovid, MD Consult, and libraries of the University of Southern California and the University of California, Los Angeles — in order to determine whether yoga can be considered a valid rehabilitation treatment for disorders like epilepsy, stroke, multiple sclerosis, peripheral nervous-system disease, fibromyalgia, and Alzheimer’s. The analysis showed that yoga did in fact demonstrate statistically encouraging physiological and psychological improvements. Yet, due to certain inadequacies in the designs of the studies they analyzed, the researchers made a call for further research to be done.
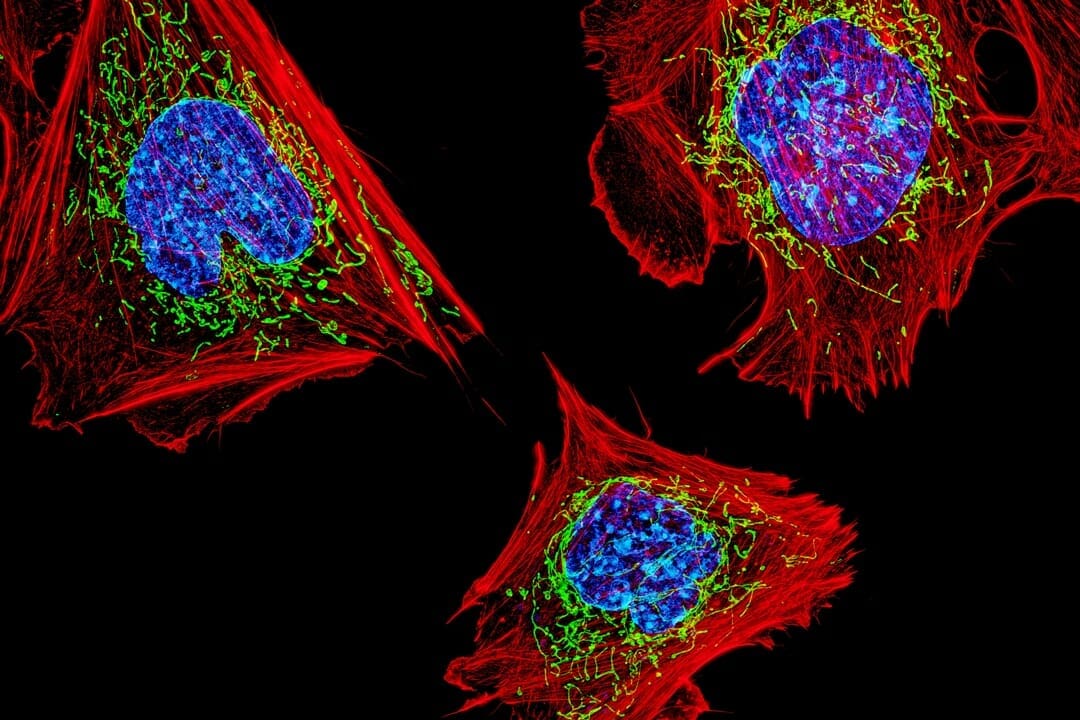
The following year, the Advanced Centre for Yoga in Mental Health and Neurosciences in Bangalore, India, answered the call and published a study in the Indian Journal of Psychiatry — one of the first studies to investigate the neurobiological effects of yoga on cortical structures in the elderly. Previous studies published from this center discovered that three months of yogasana (physical movements) and pranayama (breathing techniques) yoga therapy in adults with depression elevated the brain-derived neurotrophic factor, a neuroprotective chemical strongly expressed in the hippocampus. The hippocampus, located in the medial temporal lobe of the brain, is a very vulnerable structure that undergoes a loss of gray matter with aging. If this volume reduction is significant enough, it could be an early indicator of Alzheimer’s. Therefore, researchers hoped to see whether yoga could in fact promote an increase in the hippocampus’ volume.
Led by Dr. V.R. Hariprasad, the researchers recruited seven elderly participants (between the ages of 69 and 81) and enrolled them in a yoga program comprised of yogasana (posture), pranayama (breath control) and om (chanting) — practices that were specifically selected to provide benefits against age-related cognitive loss. When the researchers compared functional MRI scans of the seven elderly participants before and after six months in the yoga training program, they found a significant increase in bilateral hippocampus volume (in the posterior region).